 | ||||||||||
News Updates | July 23, 2015
| ||||||||||
About Acknowledgement and End-to-End Testing
While ICD-10 is almost here, you still have time to get ready. But you must get ready now. Each day this week we are highlighting 1 of the 5 recommendations to help you begin testing:
1) Why Test Now, 2) How to Get Started, 3) Testing with Trading Partners, 4) Types of Testing, and 5) Testing Tips.
Today our focus is:
Type of Testing 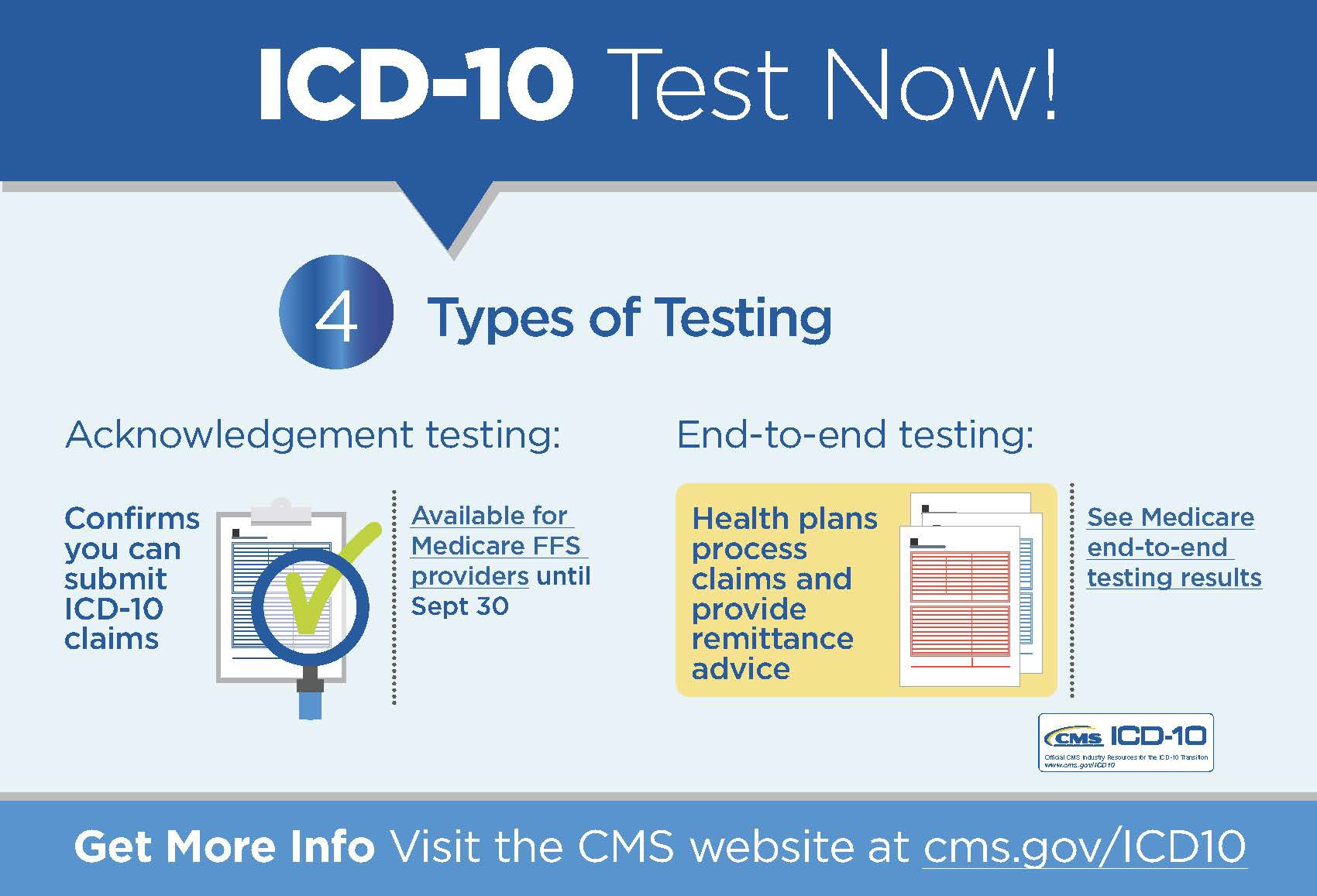
Acknowledgement Testing
Tip: Be sure to use ICD-10 qualifiers, which differ from ICD-9 qualifiers. Some providers have reported that ICD-10 qualifiers had to be manually set up in their systems.In acknowledgement testing, providers and other submitters, like clearinghouses, submit claims with ICD-10 codes and ICD-10 companion qualifiers. While claims are not adjudicated, submitters receive an acknowledgement that their claim was accepted or rejected. Beyond testing with Medicare as described below, you can check with your commercial health plans, clearinghouses, and billing services for more acknowledgement testing opportunities. Medicare FFS Acknowledgement Testing All Medicare fee-for-service (FFS) providers who submit electronic claims can conduct acknowledgement testing with their Medicare Administrative Contractor (MAC) at any time untilSeptember 30:
To submit claims for testing, you must use:
Analysis of acknowledgement testing to date has found no issues with Medicare systems for FFS claims. Rejected claims have been largely due to improperly prepared test claims—issues unrelated to ICD-10. Specific issues have been:
End-to-End Testing
While registration has closed for the Medicare FFS end-to-end testing described below, some health plans continue to offer opportunities. If you have not conducted end-to-end testing yet, check with your health plans, clearinghouses, and billing services about opportunities.During end-to-end testing, providers submit claims containing valid ICD-10 codes. Health plans process the claims through system edits to return an electronic remittance advice (ERA).
Medicare FFS End-to-End Testing
Results from the July will be analyzed and released next month.Medicare’s last round of end-to-end testing is taking place this week, ending tomorrow, July 24. Advance registration was required to participate. Medicare FFS end-to-end testing is no longer open to new volunteers. (Please note that volunteers who took part in the January or April end-to-end testing are able to participate in the current testing, even if they did not register for July). Results from the last round of Medicare FFS end-to-end testing, held April 27 to May 1, showed that overall, participants were able to successfully submit ICD-10 test claims and have them processed through the Medicare billing systems. Testers included providers, clearinghouses, and billing agencies. CMS was able to accommodate most volunteers, representing a broad cross-section of provider, claim, and submitter types. The acceptance rate for April was higher than for January, with an increase in test claims submitted and a decrease in the percentage of errors related to either ICD-9 or ICD-10 codes:
To learn more about getting ready, visit cms.gov/ICD10 for free resources including the Road to 10 tool designed especially for small and rural practices, but useful for all health care professionals.
Keep Up to Date on ICD-10Visit the CMS ICD-10 website and Roadto10.org for the latest news and resources to help you prepare. Sign up for and CMS ICD-10 Industry Email Updates and follow us on Twitter.
| ||||||||||
 |  |  | ||||||||
 |
|  | ||||||||
Friday, July 24, 2015
ICD-10 News: Types of Testing
Subscribe to:
Post Comments (Atom)
No comments:
Post a Comment